Claim Rejection Notifications

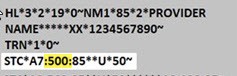
Review the various errors below to understand how to correct and resubmit. When viewing your 277CA, all TRICARE Prime® Demo by CareSource Military & Veterans™ rejections will have a Claim Status Category Code of A7. The second code is the Claim Status Code. This is the Error Number from the list below. You can find this after the A7 in the STC segment of your 277CA.
Error Number: 21
Error Description: Invalid birth weight
How to Fix: Enter a numeric birth weight.
Error Number: 21
Error Description: Newborn Delivery Claims without gestation age
How to Fix: On professional claims, the CPT procedure codes must be tied to the appropriate ICD-10 diagnosis codes. Diagnosis code validation edits on professional claims are based on detail-level diagnosis pointers, and the 5010 X12 837P standard only allows up to four diagnoses to be pointed per detail. If the weeks of gestation code is missing or not pointed to on one of the four diagnosis pointer fields in the delivery detail of the claim, the delivery detail will be denied.
Error Number: 30
Error Description: Beneficiary mismatch
How to Fix: Either the beneficiary had the wrong sex identified on the claim submission, or the beneficiary’s address on the claim does not match the beneficiary’s address in our system. Correct the data and send a new claim.
Error Number: 33
Error Description: Beneficiary not found for submitted beneficiary ID, beneficiary Mismatch, or Claim received for group not valid to process claims
How to Fix: The system will check the beneficiary ID, DOD ID (if supplied), sex, DOB, and first 4 characters of the last name to attempt to identify the correct beneficiary. Contact Provider Services at 1-800-488-0134 to resolve this issue
Error Number: 128
Error Description: Submitted Provider Tax ID not in Facets
How to Fix: The provider is not set up with CareSource to send electronic claims. The provider needs to submit a W-9 form to CareSource prior to sending electronic claims. Please contact Provider Services at 1-800-488-0134 or visit https://www.caresource.com/providers/ for instructions.
Error Number: 132
Error Description: Missing/Invalid Medicaid ID for Atypical Provider
How to Fix: Ensure correct Medicaid ID is provided.
Error Number: 187
Error Description: Date of Service (DOS) after received date
How to Fix: DOS must be prior to Received Date.
Error Number: 255
Error Description: Rejection for Newborn Delivery Claims without gestation age
How to Fix: Include Newborn Gestation age.
Error Number: 453
Error Description: Procedure code/mod combo not valid
How to Fix: Resubmit with a valid Procedure Code and/or Modifier.
Error Number: 488
Error Description: Invalid Diagnosis code
How to Fix: Enter valid Diagnosis Code(s) for services rendered.
Error Number: 508
Error Description: ICD-09 Code Found After ICD-10 Implementation Date
How to Fix: Remit current ICD-10 code.
Error Number: 538
Error Description: Corrected claim, with no original claim ID
How to Fix: If you are sending a corrected claim with frequency of 7, you must include the last adjudicated Claim ID in the REF*F8 segment.
If the last adjudicated claim ID is unknown, contact Provider Services at 1-800-488-0134.
Error Number: 677
Error Description: Rendering National Provider Identifier (NPI) not affiliated to the billing agencies
How to Fix: Rendering provider on the claim was not actively affiliated with the billing group on the Provider Maintenance Form (PMF) during the DOS. The provider’s affiliation status will need to be reviewed with ODM, and once updated on the PMF, the claim can be resubmitted.
Claims submitted with a DOS of March 25, 2021 going forward will deny/reject if the rendering provider was not actively affiliated with the billing group on the PMF during the DOS.
You can validate your information in the MITS system and if there are any additional questions, you can contact ODM at 1-800-686-1516.
Error Number: 700
Error Description: Claim is being rejected because it had an ICD-10 CPT code before ICD-10 was implemented in 2015. Majority of the time, the date is a typo or the code is not a valid ICD-10 code.
How to Fix: Correct DOS with date after ICD-10 was available.
Error Number: 773
Error Description: Claim is rejected for service line date spans more than a calendar year
How to Fix: Make sure all service lines are in the same calendar year.