Claim Rejection Notifications
What rejections are from your 277CA?
Review the various errors below to understand how to correct and resubmit.
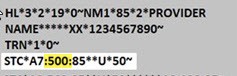
When viewing your 277CA, all CareSource rejections will have a Claim Status Category Code of A7. The second code is the Claim Status Code. This is the Error Number from the list below. You can find this after the A7 in the STC segment of your 277CA.
Error Number: 21
LOB: All
Error Description: Invalid birth weight
How to Fix: Enter a numeric birth weight.
Error Number: 21
LOB: All
Error Description: Newborn Delivery Claims without gestation age
How to Fix: On professional claims, the CPT procedure codes must be tied to the appropriate ICD-10 diagnosis codes. Diagnosis code validation edits on professional claims are based on detail-level diagnosis pointers, and the 5010 X12 837P standard only allows up to four diagnoses to be pointed per detail. If the weeks of gestation code is missing or not pointed to on one of the four diagnosis pointer fields in the delivery detail of the claim, the delivery detail will be denied.
Error Number: 30
LOB: All
Error Description: Member mismatch
How to Fix: Either the member had the wrong sex identified on the claim submission, or the member’s address on the claim does not match the member’s address in our system. Correct the data and send a new claim.
Error Number: 33
LOB: All
Error Description: Member not found for submitted member ID, HIX Member Mismatch, or Claim received for group not valid to process claims
How to Fix: The system will check the member ID, sex, DOB, and first 4 characters of the last name to attempt to identify the correct member. Contact Provider Services at 1-844-607-2831 to resolve this issue.
Error Number: 128
LOB: All
Error Description: Submitted Provider Tax ID not in Facets
How to Fix: The provider is not set up with CareSource to send electronic claims. The provider needs to submit a W-9 form to CareSource prior to sending electronic claims. Please contact Provider Services at 1-844-607-2831 or visit https://www.caresource.com/providers/ for instructions.
Error Number: 132
LOB: All
Error Description: Missing/Invalid Medicaid ID for Atypical Provider
How to Fix: Ensure correct Medicaid ID is provided.
Error Number: 187
LOB: All
Error Description: Date of Service after received date
How to Fix: Date of Service must be prior to Received Date.
Error Number: 255
LOB: All
Error Description: Rejection for Newborn Delivery Claims without gestation age
How to Fix: Include Newborn Gestation age.
Error Number: 453
LOB: All
Error Description: Procedure code/mod combo not valid
How to Fix: Resubmit with a valid Procedure Code and/or Modifier.
Error Number: 488
LOB: Al
Error Description: Invalid Diagnosis code
How to Fix: Enter valid Diagnosis Code(s) for services rendered.
Error Number: 508
LOB: All
Error Description: ICD-09 Code Found After ICD-10 Implementation Date
How to Fix: Remit current ICD-10 code.
Error Number: 538
LOB: All
Error Description: Corrected claim, with no original claim ID
How to Fix: If you are sending a corrected claim with frequency of 7, you must include the last adjudicated Claim ID in the REF*F8 segment. If the last adjudicated claim ID is unknown, contact Provider Services at 1-844-607-2831.
Error Number: 700
LOB: All
Error Description: Claim is being rejected because it had an ICD-10 CPT code before ICD-10 was implemented in 2015. Majority of the time, the date is a typo or the code is not a valid ICD-10 code.
How to Fix: Correct Date of Service with date after ICD-10 was available.
Error Number: 766
LOB: All
Error Description: Services were performed during a Health Insurance Exchange (HIX) premium payment grace period.
Error Number: 77
LOB: All
Error Description: Claim is rejected for service line date spans more than a calendar year
How to Fix: Make sure all service lines are in the same calendar year.
Error Number: 145
LOB: Indiana
Error Description: Missing the taxonomy code on the rendering provider
How to Fix: The rendering provider’s taxonomy code was not submitted on the claim; it is an Indiana Medicaid requirement that a taxonomy code be submitted for all rendering providers.
Error Number: 562
LOB: Indiana Medicaid
Error Description: Claim marked for rejection because no active provider is found in MPL based on Billing National Provider Identifier (NPI). Claims marked for rejection because there were multiple matches found in MPL based on different combinations of NPI.
How to Fix: Check status or enroll with Indiana Medicaid: https://www.in.gov/medicaid/providers/provider-enrollment/
Check status or enroll with Indiana Marketplace: https://www.caresource.com/in/providers/provider-portal/provider-maintenance/marketplace/
Error Number: 562
LOB: Indiana Medicaid
Error Description: Rendering provider not linked to billing group in Indiana MPL
How to Fix: Ensure Rendering Provider NPI is linked to the Billing Provider NPI on the Indiana Master Provider List.
Check status or enroll with Indiana Medicaid here
Error Number: 562
LOB: Indiana Medicaid
Error Description: Claim marked for rejection because the attending provider’s NPI submitted on the claim is not valid in IN MPL or not present on the claim
How to Fix: Ensure attending provider is on the claim. If the provider is on the claim, then check the attending provider NPI is valid on the Indiana Master Provider List.
Check status or enroll with Indiana Medicaid here