WE GOT YOU.
Our plans are simple and affordable with coverage for pre-existing conditions and no annual or lifetime dollar limits for essential health benefits. All plans include pediatric dental and vision benefits or coverage. You can choose to include our optional adult dental through DentaQuest®, Vision through EyeMed® and fitness benefits. So, if you need health insurance this open enrollment period, CareSource can help. We’ve been helping our members through uncertain times for over 30 years. CareSource coverage is here when you need it.
Pregnancy, maternity and newborn care
Prescription drugs
Outpatient care
Emergency services
Hospitalization
Mental health and substance use disorder services
Rehabilitative and habilitative services and devices
Laboratory services
Preventive and wellness services
Pediatric services, including dental and vision
Optional Adult Dental, Vision & Fitness benefit plans are also available.
EXTRA WAYS TO SAVE MONEY
**Four out of five customers can get a Marketplace plan for under $10 a month with financial help! **Over 70% of people who enroll in a CareSource Health Insurance Marketplace plan also qualify for a government-funded subsidy that substantially lowers the overall cost of the plan. When you enroll, you’ll see if you qualify. Eligibility for these funds is determined by the Health Insurance Marketplace, and not by CareSource. There are two ways in which the funds are distributed:
| Advance Premium Tax Credit (APTC) |
|---|
A tax credit based on income level, that lowers monthly premium payments. This can be used no matter which plan you enroll in. |
| Cost-Sharing Reduction (CSR) |
|---|
CSRs are discounts or “extra savings” that lower the amount you have to pay for deductibles, copayments, and coinsurance. CSRs only apply to Silver plans†, so if you qualify for a CSR, you must enroll in a Silver plan to get them. |
Marketplace Plan Benefits
Marketplace Plans
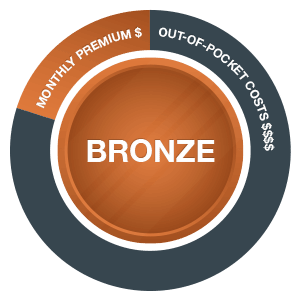
Marketplace plans are separated into metal levels of Gold, Silver, and Bronze. The metal levels are based on how you and CareSource share the cost of your health care. Note: many CareSource members are also eligible for helpful government subsidies, which will lower your cost for health care.
Are You a Member?
Get quick access to prescription coverage, find a doctor or provider, use health and educational tools, and discover what you can do with your My CareSource® account.