Find My Prescriptions
Covered Drug List (Formulary)
We call the list of prescription drugs that are covered by our plan the Formulary. Review this list with your doctor when they order drugs or supplies. There are six price tiers on the formulary. Each tier has a different cost-sharing amount, based on your plan.
Drug Formulary Changes
Drugs may be added, removed, or moved from one price tier to another. We will post these changes on our website. We will also let you know when we identify a change to our formulary that will adversely affect you.
- Summary of Formulary Changes Effective October 1, 2025
- Summary of Formulary Changes Effective July 1, 2025
- Summary of Formulary Changes Effective March 17, 2025
Price A Medication Tool
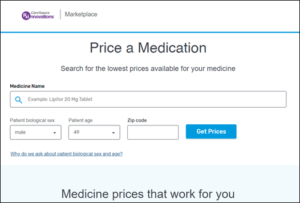
Use this tool to check coverage and get a cost estimate for prescription drugs and some supplies. This search tool is offered in partnership with Express Scripts®.
Tip: Use the tool through your CareSource MyLife account. Your specific plan information (e.g., deductible and out-of-pocket spent to date) will be used for the search, giving you a closer cost estimate.
To start your search:
- Enter your state and plan name. You can find this info on your member ID card.
- Select the type of search Price a Medication or Find a Pharmacy.
To get a price estimate for covered drugs:
- Enter the brand or generic name of the drug.
- Be sure to pick the right dose.
- The tool will show the price Tier of the drug and estimated cost. It will also tell you if prior authorization or coverage review is needed before a drug will be covered.
- If a brand name drug is not covered, the generic will show.
To check if there is a network pharmacy in your area:
- Select Find A Pharmacy.
- Enter the City/State or Zip Code to search.
Tip: If you need a prescription filled while traveling, be sure to use one of the national in-network pharmacies such a Walgreens.
Generic Substitution and Therapeutic Interchange
Generic drugs are as safe and effective as the brand name drug, as stated by the federal Food and Drug Administration (FDA). Your pharmacy may dispense a generic drug instead of a brand name drug unless your doctor directs them to dispense the brand name as written.
- Tier 1 / Generic drugs – Use generic drugs to help lower out-of-pocket costs. Brand name drugs will often be removed from the Formulary when a generic becomes available. If you or your doctor believe that you need a brand name drug when a generic is available, your doctor will need to give us more info to explain why.
- Tier 2 / Preferred – Not all brand name drugs have a generic version. Tier 2 preferred brand name drugs often have lower copays than non-preferred brand name drugs.
- Tier 3 / Non-Preferred – Many drugs in Tier 3 have lower-cost choices in Tier 1 & 2.
How to Ask For a Drug not on the Formulary
There may be a time when you may need a drug that is not on the formulary. You or your representative (including your Doctor) can ask for an exception to the formulary. If approved, the drug will be covered. Your deductible and copay or coinsurance will still apply, based on your plan. Fill out the online Member Exception Request for Non-Formulary Medication. You can also call Member Services to make the request.
If needed, CareSource will reach out to your doctor to get all the information needed. We will provide a decision no later than 72 hours after the request is received, or within 24 hours if the member is suffering from a serious health issue. Doctors may be asked to give written clinical records to show why an exception is needed. In deciding whether an exception will be given, CareSource will keep in mind whether the asked for drug is clinically appropriate.
Drug Safety Recalls
Sometimes, the federal government issues drug recalls. To find out if a drug you take is being recalled, please check the listings on the U.S. Food & Drug Administration website.