Understanding Your Costs
Cost Sharing
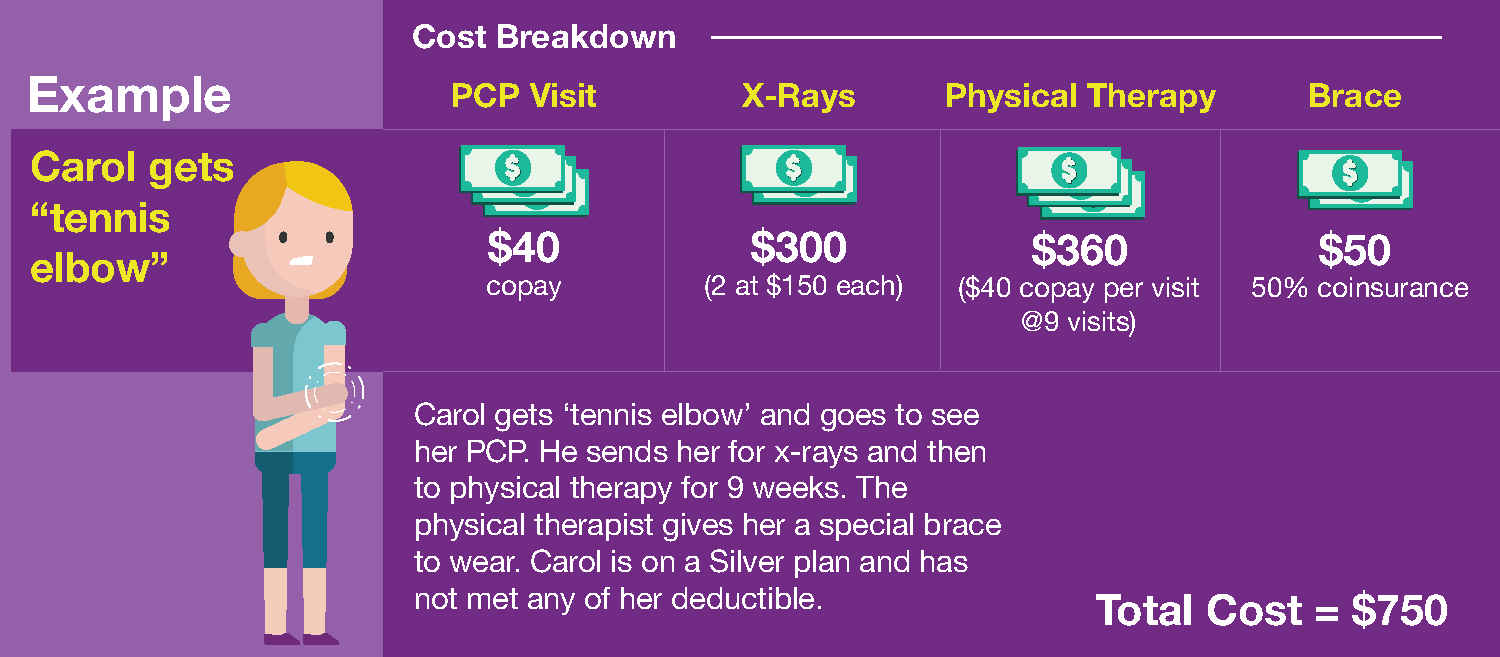
The amount you pay out of pocket for care and services. It defines how you and CareSource will share the cost of your care. Copayment, coinsurance and deductible are types of cost sharing. To see the cost-sharing requirements for your plan, see the Schedule of Benefits and Summary of Benefits and Coverage.
Copayment (Copay)
A fixed amount you pay for when you receive certain covered services. It is paid by you whether or not your deductible has been met. Your copay changes based on where you get care, the type of provider you use, and the service received. For example, your PCP will have a lower copay than a specialist. If you have multiple lab tests done, a copay will apply per test.
Coinsurance
A percentage of the cost for an in-network service. It is normally paid after your deductible has been met.
Deductible
The amount you pay towards your in-network health care costs before your plan begins to assist with the cost.
Maximum Out of Pocket (MOOP)
The most you have to spend on in-network covered care or services during any plan year before CareSource pays 100%. The MOOP does not include any non-covered or excluded care and services.
Premium
The monthly cost for your insurance policy. You must pay premium monthly regardless of services used.
Billed Amount
The amount that your provider charges for the services they provide. It can influence the amount you have to pay. If you go to a provider who charges more for services than others, the portion you have to pay may be higher if the services you get are subject to deductible or coinsurance. You will see this on your Explanation of Benefits (EOB). You can also view claims info in CareSource MyLife.
In-Network
We have contracted rates with providers who you are able to see for health care services. Covered services received from in-network providers apply to your plan benefits. We negotiate rates with our network providers to keep costs low. It also helps make sure you get high quality care and respect for your rights as a member.
Out-of-Network
A provider who is not in our contracted network. If you are treated by an out-of-network provider without pre-approval, the services will not apply to your plan benefits, except in an emergency. You may also be subject to balance billing from that provider to cover the amount that CareSource was not allowed to pay. If you think you need care from an out-of-network provider, please call Member Services at 1-877-514-2442 (TTY: 711).
Marketplace
A place where individuals, families, and small businesses can browse health plans and prices and enroll in coverage in their area. CareSource plans are available on the federal Health Insurance Marketplace (Exchange) at Healthcare.gov. It was established by the Affordable Care Act (ACA).
Advance Premium Tax Credit (APTC)
A subsidy that your insurer receives on your behalf from the federal government to lower monthly premium responsibility. APTC eligibility is based on your expected household income for the plan year. APTC can change when your income changes. You can only get an APTC if you apply for coverage through the Health Insurance Marketplace® (Exchange) at Healthcare.gov.
Plan Documents
The member materials that explain your health plan. These include your Certificate of Coverage, Schedule of Benefits, and Summary of Benefits and Coverage.
Need more definitions?